Introduction
Handling sensitive patient information requires more than just best practices—it’s a legal requirement. The Health Insurance Portability and Accountability Act (HIPAA) sets the standards for how organizations must manage and secure health information. Staying compliant isn’t just about avoiding fines; it’s about protecting patient trust and ensuring their data is kept safe.
What is HIPAA?
HIPAA, which stands for the Health Insurance Portability and Accountability Act, enacted in 1996, is a set of regulations designed to secure protected health information (PHI) and ensure that healthcare providers handle patient data responsibly. It covers privacy, security, and breach notification requirements that apply to anyone who handles patient records, including healthcare providers and their partners.
A critical part of HIPAA compliance is the Business Associate Agreement (BAA). This contract is essential when healthcare providers work with third-party vendors who have access to PHI. The BAA ensures that these vendors are also following HIPAA standards. Without it, healthcare providers can be held liable for data breaches caused by these partners.
Read more about HIPAA’s legal requirements from the Department of Health and Human Services.
Why HIPAA Compliance Matters
For healthcare providers, non-compliance carries significant risks. Fines for violations can range from $100 to $50,000 per incident, depending on the level of negligence. Beyond financial penalties, a breach can damage an organization’s reputation, erode patient trust, and disrupt operations.
HIPAA compliance ensures that sensitive information, including medical records and personal data, is handled securely. Compliance not only helps healthcare organizations avoid fines but also strengthens their ability to protect patient information in an increasingly digital world.
Explore Tadabase's HIPAA features.
Challenges in Managing HIPAA Compliance
Maintaining HIPAA compliance can be complex, especially when working with digital records and multiple data systems. The main challenges include:
- Data Security: Patient information must be safeguarded against breaches and unauthorized access.
- Access Control: Not everyone needs full access to patient data. Proper role-based permissions are essential.
- Audit Requirements: Every interaction with patient data must be logged to ensure accountability.
- Backup and Recovery: HIPAA requires that data be backed up securely and recoverable in the event of a system failure or breach.
Without a robust system to manage these areas, healthcare providers run the risk of non-compliance.
HIPAA-Compliant Features for Data Management
A HIPAA-compliant platform should include the following features to ensure that patient information is always secure:
Encryption
HIPAA requires encryption to protect sensitive data. Whether it’s stored or transmitted, encryption ensures that unauthorized users cannot access or read the information.
Access Controls
Role-based access allows organizations to restrict who can view or modify patient information. By limiting access to authorized personnel, healthcare providers reduce the risk of breaches.
Audit Logs
HIPAA mandates that all interactions with patient data are logged. These detailed audit logs help healthcare organizations track who accessed information and what changes were made, ensuring full transparency.
Regular Backups
HIPAA compliance requires regular, secure backups. In the event of a system failure or cyberattack, these backups ensure that patient data can be restored quickly without violating compliance standards.
How HIPAA Compliance Fits Into Daily Operations
For many healthcare organizations, compliance can feel like a burden. However, building compliance into the day-to-day workflow simplifies the process and minimizes risk. A well-designed platform should make it easy to maintain HIPAA standards without disrupting regular operations.
Here’s how compliance can be integrated into a healthcare provider’s workflow:
- Customizable Permissions: Define roles for each user, ensuring they have access only to the information necessary for their job.
- Automated Logs: Automatically track all interactions with patient data, eliminating the need for manual monitoring.
- Secure Transfers: Ensure that data being shared between departments or systems is encrypted and protected from unauthorized access.
- Disaster Recovery Plans: Schedule regular backups of patient data, ensuring that in the event of a breach, the information can be restored without compromising compliance.
When HIPAA compliance is built into daily operations, it becomes a natural part of the process rather than an additional burden.
How Tadabase Saved Aeris Medical $180K with HIPAA Compliance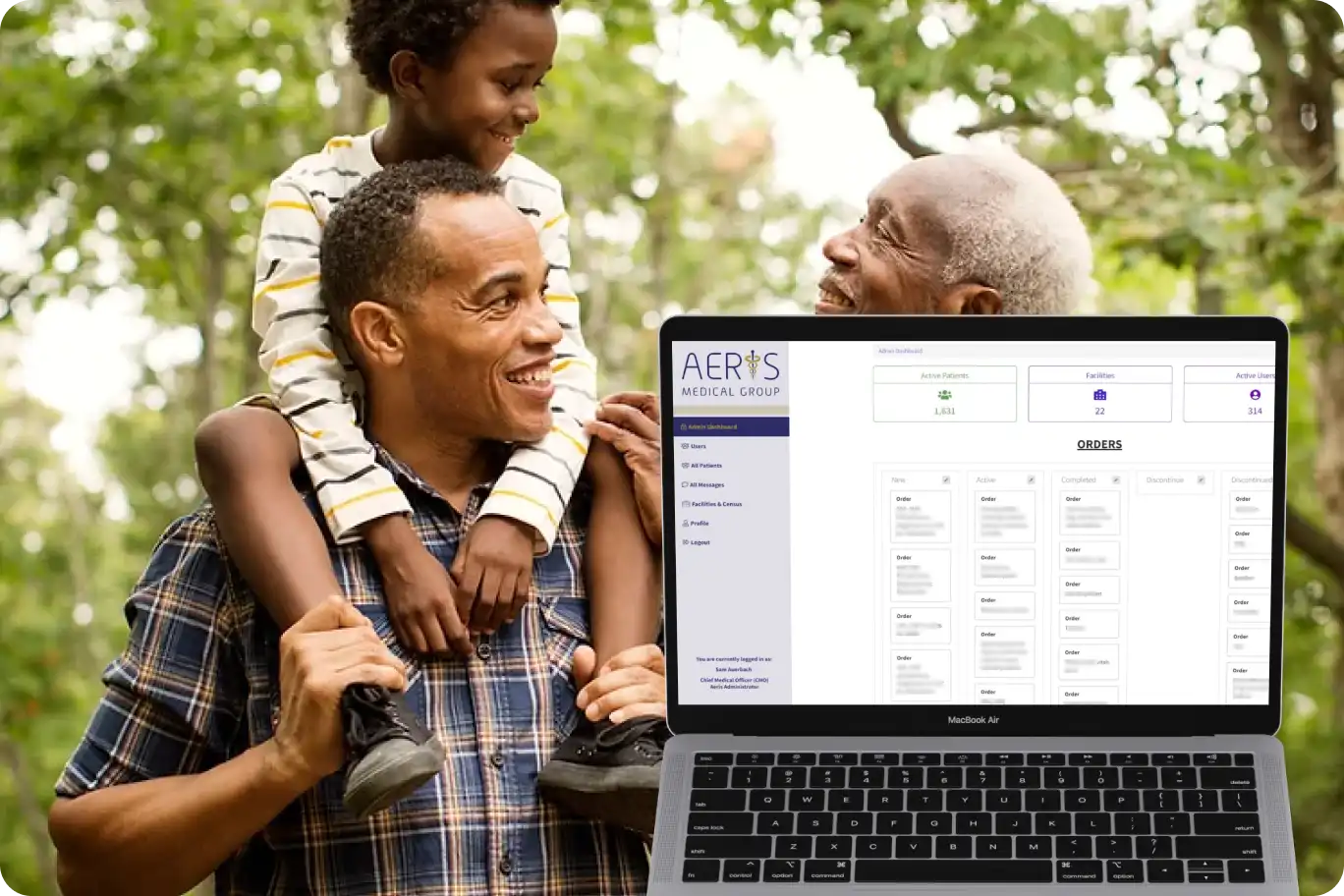
Aeris Medical Group, a mid-sized healthcare provider, struggled with managing patient data across multiple disconnected systems. With one platform for scheduling, another for medical records, and a third for billing, maintaining control over sensitive information was becoming difficult. Staff had inconsistent access to patient data, and there were concerns about how securely the information was being managed.
After adopting a HIPAA-compliant platform, Aeris Medical Group saw immediate improvements:
- Centralized Data Management: All patient information, from billing to medical records, was consolidated into one secure system.
- Role-Based Access: Permissions were customized based on each staff member’s role, ensuring that sensitive data could only be accessed by authorized personnel.
- Detailed Audit Logs: Every interaction with patient data was automatically tracked, making compliance audits much simpler.
- Regular Backups: Secure, encrypted backups were implemented to ensure data could be recovered in case of a disaster or system failure.
By switching to a unified, HIPAA-compliant platform, Aeris Medical Group improved both data security and operational efficiency.
Learn more about Aeris Medical Group’s transformation here.
HIPAA Compliance Checklist
Healthcare providers can use the following checklist to ensure they are meeting HIPAA requirements:
Encrypt Data: Ensure that all patient data, both at rest and in transit, is encrypted to protect against unauthorized access.
Implement Access Control: Limit access to sensitive data through role-based permissions.
Maintain Audit Logs: Keep detailed records of all interactions with patient data, including access and changes made.
Backup Regularly: Have secure, encrypted backups in place to restore patient data in the event of a breach or failure.
Use Business Associate Agreements (BAAs): Make sure all third-party vendors handling patient data have signed BAAs to ensure they are HIPAA-compliant.
Plan for Breach Notifications: Develop a protocol for notifying affected individuals and authorities in case of a data breach.
This checklist helps ensure that all essential components of HIPAA compliance are addressed and integrated into daily operations.
Learn more about architecting for HIPAA on Tadabase.
FAQs on HIPAA Compliance
What is HIPAA?
HIPAA (Health Insurance Portability and Accountability Act) sets rules for protecting patient health information. It includes standards for privacy, security, and breach notifications.
What is a BAA?
A Business Associate Agreement (BAA) is a contract that requires third-party vendors handling patient data to comply with HIPAA standards. Without a BAA, healthcare providers are responsible for any breaches caused by those vendors.
How does encryption help with HIPAA compliance?
Encryption ensures that sensitive patient data remains unreadable to unauthorized individuals, even if they gain access to the information.
What happens if my organization isn’t HIPAA compliant?
Non-compliance can result in significant fines, legal consequences, and loss of patient trust. HIPAA violations can incur fines ranging from $100 to $50,000 per incident, depending on the severity.
Key Takeaways for Healthcare Providers
Staying HIPAA-compliant doesn’t have to be overwhelming. Focus on these key areas to ensure compliance:
- Data Security: Encryption and role-based access control are critical to protecting sensitive data.
- System Integration: A centralized platform simplifies the process of managing patient data securely.
- Audit Logs: Keep detailed logs of every interaction with patient information to ensure accountability and transparency.
- Disaster Recovery: Implement regular backups to ensure data can be restored quickly and securely in the event of a breach.
By adopting the right tools and workflows, healthcare providers can ensure compliance while focusing on delivering high-quality care to their patients.